- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer
Attention-Deficit/Hyperactivity Disorder (ADHD)
Attention-Deficit/Hyperactivity Disorder (ADHD)
ADHD
The introduction to the article on Attention-Deficit/Hyperactivity Disorder (ADHD) provides an overview of this neurodevelopmental disorder, encompassing its symptoms of inattention, hyperactivity, and impulsivity. It outlines the prevalence and historical context of ADHD while emphasizing its significance. The introduction sets the stage for exploring the disorder’s complexities, diagnostic criteria, underlying causes, and the diverse range of treatments and interventions available to enhance the quality of life for individuals affected by ADHD.
Symptoms and Diagnostic Criteria

Inattention Symptoms
Inattention symptoms characterize one facet of Attention-Deficit/Hyperactivity Disorder (ADHD), involving difficulties sustaining focus, organizing tasks, and following through on responsibilities. Individuals may struggle with avoiding distractions, frequently making careless mistakes, and forgetting daily obligations. These symptoms can impact academic, occupational, and personal functioning, underscoring the need for comprehensive assessment and tailored interventions to address the challenges posed by inattention in individuals with ADHD.
Hyperactivity Symptoms
Hyperactivity symptoms constitute a core element of Attention-Deficit/Hyperactivity Disorder (ADHD), manifesting as excessive restlessness, fidgeting, and an inability to remain seated or engaged in quiet activities. Individuals may display impulsive actions, difficulty awaiting turns, and a heightened tendency to interrupt others. These symptoms can lead to disruptions in social interactions and academic settings, necessitating targeted strategies and treatments to manage hyperactivity and enhance overall well-being in individuals with ADHD.
Impulsivity Symptoms
Impulsivity in ADHD encompasses rash decision-making, difficulty curbing immediate desires, and acting without forethought. Individuals may exhibit impulsive speech, interruptions, and a tendency to engage in risky behaviors. These symptoms can disrupt social interactions, academic progress, and personal goals. Managing impulsivity involves targeted interventions like cognitive-behavioral therapy and medication, aiming to improve self-control, enhance decision-making, and promote more adaptive behaviors in individuals grappling with ADHD.
Diagnostic Criteria According to DSM-5
The Diagnostic and Statistical Manual of Mental Disorders (DSM) outlines criteria for diagnosing ADHD. It requires persistent patterns of inattention, hyperactivity, and impulsivity, leading to functional impairments. Symptoms must be present for at least six months, evident in multiple settings, and not solely explained by another condition. The DSM provides guidelines to distinguish between the three ADHD presentations (predominantly inattentive, hyperactive-impulsive, and combined) and aids clinicians in accurate diagnosis and appropriate healthcare treatment planning.
Causes and Risk Factors

Genetic Factors
Genetic factors play a substantial role in the development of ADHD. Studies involving family and twin research have highlighted a hereditary component, suggesting that genes contribute to susceptibility. Specific genes related to neurotransmitter regulation, dopamine signaling, and neural development have been implicated. While genetics increase vulnerability, environmental interactions also play a role. Understanding the interplay between genetic predisposition and environmental influences can enhance insights into ADHD’s origins and potential treatment strategies.
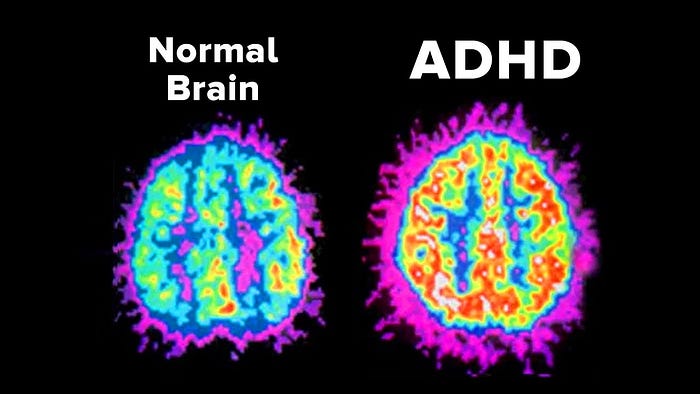
Neurobiological Factors
Neurobiological factors contribute significantly to ADHD’s manifestation. Neuroimaging studies reveal structural and functional differences in brain regions involved in attention, impulse control, and executive functions. Reduced prefrontal cortex activity, altered dopamine signaling, and disrupted neural pathways have been observed. These factors contribute to attention and behavioral challenges. A comprehensive understanding of these neurobiological underpinnings aids in formulating targeted interventions and therapies for individuals with ADHD.
Environmental Factors
Environmental factors also influence ADHD development. Prenatal exposure to toxins like tobacco and alcohol, premature birth, low birth weight, and maternal stress can increase risk. Early childhood adversity, disrupted family dynamics, and limited access to educational resources may exacerbate symptoms. While genetics set the stage, environmental interactions contribute significantly. Recognizing and addressing these factors are crucial for a holistic understanding of ADHD and tailoring effective intervention approaches.
Potential Role of Brain Structure and Function
Brain structure and function are key contributors to ADHD. Neuroimaging reveals differences in brain regions related to attention and impulse control. Reduced gray matter volume in the prefrontal cortex and abnormalities in the basal ganglia and cerebellum are observed. Dysregulation of neurotransmitter systems, particularly dopamine, affects signal transmission. These structural and functional variances underpin ADHD symptoms and guide research into targeted interventions that could normalize brain activity and alleviate cognitive challenges.
Types of ADHD
ADHD Predominantly Inattentive Presentation
ADHD Predominantly Inattentive Presentation, a subtype of ADHD, is characterized by persistent inattention, difficulty sustaining focus, and poor organization. Individuals may struggle with details, overlook instructions, and have trouble completing tasks. Unlike hyperactivity, restlessness is less pronounced. This presentation can affect academic performance and daily functioning. Accurate assessment and tailored interventions, such as behavior therapy and educational accommodations, help address these challenges and enhance quality of life.
ADHD Predominantly Hyperactive-Impulsive Presentation
ADHD Predominantly Hyperactive-Impulsive Presentation, a variant of ADHD, involves excessive hyperactivity and impulsivity. Individuals may fidget, squirm, and struggle to stay seated. Impulsiveness leads to hasty decisions, interruptions, and difficulty waiting turns. This presentation may hinder social interactions and academic progress. Diagnosis entails persistent symptoms, with treatment often including behavioral interventions and, in some cases, medication. Targeted approaches address hyperactivity and impulsivity, promoting better functioning and well-being.
ADHD Combined Presentation
ADHD Combined Presentation is a prevalent form of the disorder, encompassing both inattention and hyperactivity-impulsivity symptoms. Individuals experience difficulty focusing, organizing tasks, and exhibit restlessness and impulsiveness. This presentation poses challenges across academic, social, and personal domains. Comprehensive assessment is vital, and treatment typically involves a combination of behavioral strategies, therapy, and sometimes medication. Tailored interventions address the dual nature of symptoms, aiming to improve overall functioning and quality of life.
Coexisting Conditions and Comorbidities
ADHD often coexists with various comorbidities, compounding its impact. Learning disabilities, such as dyslexia or dyscalculia, frequently accompany ADHD, exacerbating academic struggles. Oppositional Defiant Disorder and Conduct Disorder manifest as defiant or aggressive behavior. Anxiety and mood disorders, like depression, intensify emotional challenges. Autism Spectrum Disorder may overlap, complicating social interactions. Addressing these coexisting conditions requires a holistic approach, combining interventions tailored for each disorder. Comprehensive assessment, collaborative healthcare treatment planning, and a nuanced understanding of the interactions between ADHD and its comorbidities are essential for effective management and improved well-being in individuals with multiple challenges.
Assessment and Diagnosis
Assessment and diagnosis of ADHD involve a comprehensive process. Clinical interviews with the individual and family, along with behavior rating scales, contribute to a thorough evaluation. Differential diagnosis ensures distinguishing ADHD from other conditions with similar symptoms. A multidimensional approach considers behavioral, cognitive, and emotional aspects, across various settings. Accurate diagnosis aids in personalized intervention planning, including behavioral strategies, psychoeducation, and, if necessary, medication. Ongoing monitoring and reevaluation are vital for tracking progress and adjusting interventions. A comprehensive assessment framework enables effective identification and management of ADHD, promoting optimal functioning and improving quality of life.
Treatment Approaches
ADHD treatment employs diverse approaches. Behavioral interventions, including parent training and behavioral modification, enhance coping skills and self-regulation. Pharmacological options, such as stimulant and non-stimulant medications, target symptom control. Psychotherapy, like Cognitive-Behavioral Therapy and social skills training, fosters adaptive behaviors. Multimodal treatment combines strategies for a holistic approach. Individualized educational plans and classroom accommodations support academic success. Lifestyle strategies, like time management and mindfulness, improve daily functioning. Lifespan considerations ensure tailored interventions for children, adolescents, and adults. Comprehensive treatment addresses various dimensions of ADHD, enabling symptom management, skill development, and improved overall well-being.
Coping Strategies and Lifestyle Management

Coping strategies and lifestyle management are crucial for individuals with ADHD. Time management techniques, organization skills, and setting priorities aid in task completion. Mindfulness and relaxation exercises enhance focus and emotional regulation. Maintaining a balanced routine, regular exercise, and adequate sleep contribute to overall well-being. Establishing supportive routines and seeking social connections provide stability. Effective communication skills and stress management techniques bolster relationships. Adapting environments to reduce distractions and setting realistic goals aid daily functioning. Utilizing these strategies, individuals can cultivate resilience, optimize their strengths, and navigate challenges associated with ADHD, leading to improved quality of life and self-empowerment.
Lifespan Considerations

ADHD’s impact evolves across the lifespan. Children may face academic challenges, while adolescents grapple with impulsivity and risky behaviors. In adults, symptoms can affect relationships, work performance, and self-esteem. Tailored interventions and coping strategies should evolve accordingly. Early intervention for children and adolescents is crucial for skill development. For adults, strategies to manage responsibilities, maintain focus, and enhance interpersonal skills are essential. Recognizing ADHD’s changing manifestations guides effective support throughout different life stages, fostering long-term success and well-being.
Myths and Misconceptions About ADHD
Myths and misconceptions surrounding ADHD contribute to misunderstanding and stigma. Some believe ADHD is merely a result of laziness or lack of discipline, disregarding its neurobiological basis. Others assume it only affects children, neglecting the prevalence in adults. Qme Healthcare System Software plays a vital role in dispelling these myths. Through accurate data collection, streamlined communication, and comprehensive patient records, Qme Healthcare System Software helps healthcare professionals make precise ADHD diagnoses, educate patients and families about the condition, and provide tailored treatment plans. By integrating technology, Qme Healthcare System Software enhances awareness, challenges misconceptions, and facilitates effective ADHD management.
Current Research and Future Directions
Current research in ADHD delves into neurobiological mechanisms, genetic factors, and comorbidities. Future directions emphasize personalized treatments, precision medicine, and digital health interventions. Qme Healthcare System Software plays a pivotal role by facilitating data collection, streamlining patient information, and supporting remote monitoring. Its integration empowers researchers to analyze large datasets, refine treatment approaches, and develop innovative strategies. Qme Healthcare System Software role extends to enhancing telehealth services, fostering cross-disciplinary collaborations, and contributing to the evolution of ADHD research and care paradigms, ultimately improving outcomes for individuals affected by the disorder.
Conclusion
In conclusion, our understanding of ADHD has grown significantly, dispelling myths and highlighting the complex interplay of genetic, neurobiological, and environmental factors. The evolving landscape of research offers promising avenues for personalized treatments and improved patient outcomes.
Qme Healthcare System Software stands as a valuable asset in this journey. Its seamless integration with clinical practice and research endeavors has streamlined data collection, enhanced patient care, and facilitated collaborative efforts. By providing a robust platform for comprehensive patient information, telehealth services, and research support, QMe healthcares contributes to advancing ADHD knowledge, promoting evidence-based interventions, and ultimately fostering a brighter future for individuals grappling with this condition. As research continues to evolve, QMe remains at the forefront, playing a crucial role in shaping the trajectory of ADHD care and research.
- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer