- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer
BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE.

URINARY INCONTINENCE: A DETAILED ANALYSIS
Urinary incontinence is a medical condition in which a person has trouble controlling their bladder, causing unintentional leakage of urine. This means that they might have accidents and leak urine when they don’t want to. Urinary incontinence can be temporary or ongoing, and it can affect people of all ages. This condition can range in severity, from occasional minor leaks to a complete loss of bladder control.It can happen due to various reasons, like weak pelvic muscles, nerve problems, or certain health conditions.
There are different types of urinary incontinence, including:

-
Stress Incontinence: This type of incontinence occurs when pressure is placed on the bladder, such as during coughing, sneezing, laughing, or lifting heavy objects, causing small amounts of urine to leak.
-
Urge Incontinence: Also known as “overactive bladder,” this type involves a sudden and strong urge to urinate, followed by involuntary urine leakage. The person may not make it to the bathroom in time.
-
Overflow Incontinence: In this type, the bladder doesn’t empty completely, leading to constant dribbling or leakage of small amounts of urine.
-
Mixed Incontinence: Some individuals may experience a combination of stress and urge incontinence.
The impact of urinary incontinence can be significant, affecting a person’s quality of life, confidence, and emotional well-being. However, it’s essential to know that urinary incontinence is a treatable condition.
If someone experiences urinary incontinence, it’s crucial to seek medical evaluation and support from a healthcare professional. This article focuses on the causes, symptoms and treatment of urinary incontinence. QMe offers packages support for various medical services and features automated billing to ensure transparent and hassle-free financial transactions. Embracing QMe empowers hospitals to enhance patient experiences, optimize healthcare workflows, and deliver top-notch medical services
CAUSES LEADING TO URINARY INCONTINENCE
Urinary incontinence can have various underlying causes. Some of the common factors contributing to the condition may include:
1.Weak Pelvic Muscles: The muscles that support the bladder and control urine flow may become weakened due to factors like pregnancy, childbirth, aging, or certain medical conditions.
-
Nerve Damage: Conditions that affect the nerves controlling the bladder, such as diabetes, multiple sclerosis, stroke, or spinal cord injuries, can lead to urinary incontinence.
-
Hormonal Changes: Changes in hormone levels, particularly during menopause, can affect the urinary system and contribute to incontinence.
-
Urinary Tract Infections (UTIs): Infections in the urinary tract can irritate the bladder and cause temporary incontinence.
-
Certain Medications: Some medications, like diuretics or drugs that relax the bladder muscles, may contribute to urinary incontinence as a side effect.
-
Enlarged Prostate: In men, an enlarged prostate gland can obstruct the flow of urine and lead to overflow incontinence.
-
Constipation: Chronic constipation can put pressure on the bladder and contribute to stress incontinence.
-
Pelvic Organ Prolapse: A condition where the pelvic organs (such as the bladder, uterus, or rectum) descend into the vagina, possibly causing stress incontinence.
-
Obstruction or Tumors: Any obstruction or growths in the urinary tract can interfere with normal bladder function and lead to incontinence.
-
Neurological Disorders: Conditions like Parkinson’s disease or Alzheimer’s disease can affect the brain’s control over bladder function.
These are the causes that lead to urinary incontinence and by opting right treatment it can rehabilitate and a person can lead a healthy life. Early diagnosis and treatment can help improve the quality of life and manage the condition effectively.QMe offers packages support for various medical services and features automated billing to ensure transparent and hassle-free financial transactions. Embracing QMe empowers hospitals to enhance patient experiences, optimize healthcare workflows, and deliver top-notch medical services.
EXPERIENCING THESE SYMPTOMS? YOU MAY BE SUFFERING FROM URINARY INCONTINENCE
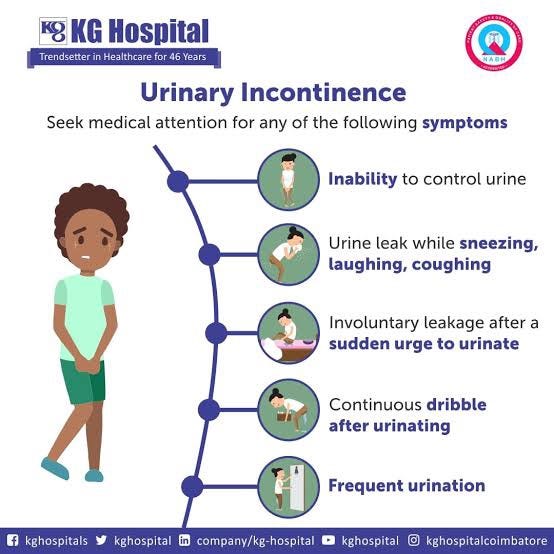
The symptoms of urinary incontinence can vary depending on the type and underlying cause of the condition. Some common symptoms include:
-
Unintentional Urine Leakage: The primary symptom of urinary incontinence is the unintentional leakage of urine. It can range from minor drops to a significant amount, depending on the severity of the condition.
-
Stress Incontinence: With stress incontinence, urine leakage may occur during activities that put pressure on the bladder, such as coughing, sneezing, laughing, lifting, or exercising.
-
Urge Incontinence: People with urge incontinence experience a sudden, strong urge to urinate and may not be able to reach the bathroom in time before urine leakage occurs.
-
Frequency: Frequent urination is another symptom, where a person feels the need to urinate more often than usual.
-
Nocturia: Nocturia refers to the need to get up multiple times during the night to urinate.
-
Overactive Bladder: Some individuals may experience a combination of urgency, frequency, and urge incontinence, known as an overactive bladder.
-
Dribbling: Continuous, slow leakage of urine, even after using the restroom, is a common symptom in certain types of incontinence.
-
Discomfort or Burning Sensation: In some cases, urinary incontinence may be associated with discomfort or a burning sensation during urination, indicating a possible urinary tract infection.
-
Emotional Impact: Urinary incontinence can lead to embarrassment, anxiety, and a negative impact on a person’s emotional well-being, affecting their social life and self-confidence.
If someone experiences any of these symptoms or suspects they may have urinary incontinence, it’s essential to seek medical evaluation and support from a healthcare professional. They can provide a proper diagnosis, identify the underlying cause, and recommend appropriate treatment options to improve urinary control and overall quality of life.
QMe is a cutting-edge hospital management software designed to revolutionize healthcare facilities worldwide. With its intelligent queue-based OPD management system, patients experience reduced waiting times and optimized appointment scheduling. The QMe software’s comprehensive patient history and electronic health records ensure seamless access to critical medical information, enabling healthcare professionals to make informed decisions and provide personalized care.
DIAGNOSED WITH URINARY INCONTINENCE? DON’T WORRY IT’S CURABLE!
Yes! You heard it right!!The treatment of urinary incontinence depends on the type and underlying cause of the condition. Some common treatment approaches include:
-
Lifestyle Modifications:
-
. – Pelvic floor exercises (Kegel exercises) can help strengthen the muscles that control bladder function.
-
. – Maintaining a healthy weight through regular exercise and a balanced diet can reduce pressure on the bladder.
-
. – Limiting fluid intake before bedtime can help reduce nighttime trips to the bathroom.
-
. – Avoiding bladder irritants such as caffeine, alcohol, and acidic or spicy foods can alleviate symptoms.
-
Behavioral Techniques:
. – Bladder training involves scheduled bathroom trips and gradually increasing the time between voiding to improve bladder control.
. – Double voiding, where the person urinates, waits a moment, and then tries to empty the bladder again, can help empty the bladder more fully.
- Medications:
. – Depending on the type of urinary incontinence, medications such as anticholinergics, beta-3 agonists, alpha-adrenergic agonists, or topical estrogen may be prescribed to manage symptoms.
- Medical Devices:
. – A pessary, a small device inserted into the vagina, can provide support to the bladder and reduce stress incontinence.
. – Urethral inserts or incontinence clamps may be used to compress the urethra and prevent urine leakage during physical activities.
- Nerve Stimulation:
. – Electrical nerve stimulation can be used to stimulate the nerves that control bladder function, helping to reduce overactive bladder symptoms.
- Injections:
. – Botox injections into the bladder muscle can help relax an overactive bladder and reduce incontinence episodes.
- Surgery:
. – Surgical procedures may be considered for certain types of urinary incontinence that do not respond to conservative treatments. Examples include sling procedures for stress incontinence or bladder neck suspension for prolapse-related incontinence.
KEGEL EXERCISES & BEHAVIOUR MODIFICATION: A DETAILED UNDERSTANDING
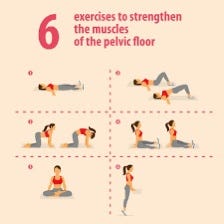
Kegel exercises, also known as pelvic floor exercises, are a set of exercises designed to strengthen the muscles of the pelvic floor.
Performing Kegel exercises involves the following steps:
STEP 1-
Identify the Muscles: To find the right muscles, try stopping the flow of urine while urinating. The muscles used to do this are the ones targeted by Kegel exercises.
STEP 2-
Empty Your Bladder: Once you have identified the pelvic floor muscles, empty your bladder to avoid any risk of infection or disruption to normal urinary function.
STEP 3-
Find a Comfortable Position: You can perform Kegel exercises while lying down, sitting, or standing, depending on your preference.
STEP 4-
Tighten and Lift: Squeeze and lift the pelvic floor muscles, as if trying to stop the flow of urine or prevent passing gas. Try to hold the contraction for 3 to 5 seconds.
STEP 5-
Relax: Release the muscles and rest for 3 to 5 seconds between contractions.
STEP 6-
Repeat: Aim for 10 to 15 repetitions per session and gradually increase the number of repetitions as you become more comfortable with the exercises.
It’s important to focus on contracting only the pelvic floor muscles without tensing the abdominal, buttock, or thigh muscles. Avoid holding your breath during the exercises.
Kegel exercises can be done throughout the day, and consistency is key to achieving results. Regular practice can help strengthen the pelvic floor muscles, improve bladder control, and reduce symptoms of urinary incontinence. It’s important to note that Kegel exercises may not be suitable for everyone, especially if there are other underlying medical conditions. If someone is unsure about performing Kegel exercises or has concerns about urinary incontinence, it’s essential to consult a healthcare professional for proper guidance and personalized advice. QMe’s automatic workflows streamline administrative tasks and treatment plans, enhancing overall efficiency and reducing human errors. The software’s IPD management feature enables smooth inpatient care coordination, while its TPA support simplifies insurance processes. Additionally, QMe offers packages support for various medical services and features automated billing to ensure transparent and hassle-free financial transactions. Embracing QMe empowers hospitals to enhance patient experiences, optimize healthcare workflows, and deliver top-notch medical services.
BEHAVIOUR MODIFICATION
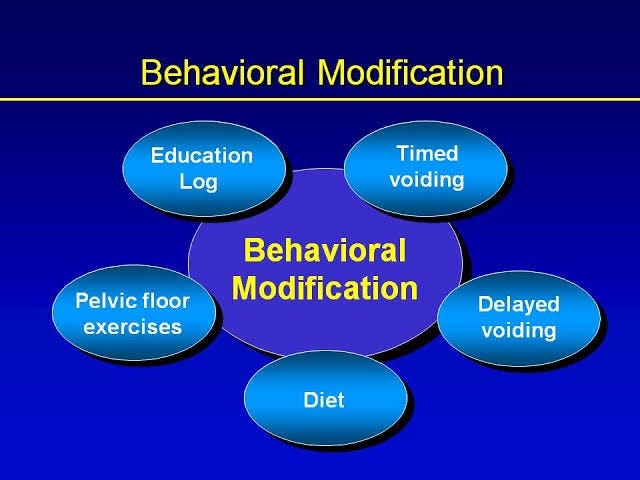
Behaviour modification is an approach used to change or manage specific behaviour through various techniques and strategies. In the context of managing urinary incontinence, behavior modification techniques can be helpful in improving bladder control and reducing the frequency of unintentional urine leakage. Some common behavior modification strategies for urinary incontinence include:
-
Bladder Training: Bladder training involves establishing a regular and timed voiding schedule. The person consciously delays urination based on a predetermined schedule, gradually increasing the time between bathroom trips. This helps to increase the bladder’s capacity and reduce the frequency of urgent and frequent urination.
-
Fluid Management: Monitoring and regulating fluid intake can help manage urinary incontinence. Reducing fluid intake before bedtime may help reduce nighttime trips to the bathroom and improve sleep quality.
-
Timed Voiding: Setting specific times for bathroom breaks, even if there is no immediate urge to urinate, can help prevent accidents and ensure the bladder is emptied regularly.
-
Avoiding Bladder Irritants: Certain foods and drinks can irritate the bladder and contribute to incontinence. Avoiding or limiting caffeine, alcohol, carbonated beverages, and acidic or spicy foods may help alleviate symptoms.
-
Double Voiding: After urinating, trying to empty the bladder again after waiting a moment can help ensure the bladder is emptied more completely, reducing the risk of residual urine leakage.
-
Prompt Response: Responding promptly to the urge to urinate and not holding back when the need arises can prevent overfilling of the bladder and improve bladder control.
-
Pelvic Floor Exercises: Including pelvic floor exercises (Kegel exercises) as part of behavior modification can help strengthen the muscles that control urinary function and improve bladder control.
PREVENTATIVE MEASURES
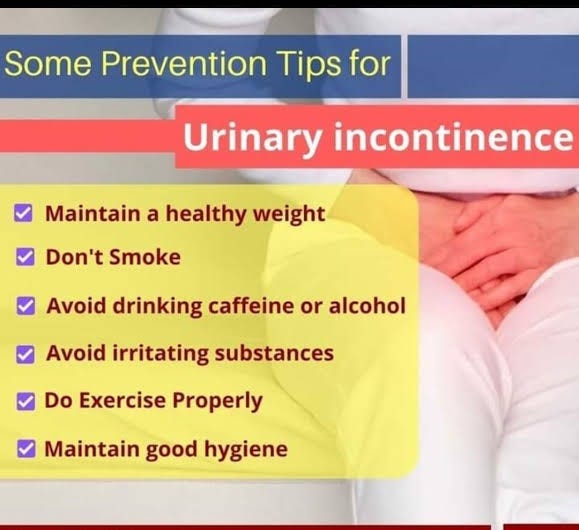
While there is no surefire way to completely prevent urinary incontinence, there are some lifestyle changes and practices that may help reduce the risk of developing the condition or improve urinary control in those experiencing mild symptoms. Here are some prevention strategies:
-
Pelvic Floor Exercises: Regularly performing pelvic floor exercises (Kegel exercises) can help strengthen the muscles that support the bladder and improve bladder control. These exercises are beneficial for both preventing and managing urinary incontinence.
-
Maintain a Healthy Weight: Excess weight can put additional pressure on the bladder and pelvic muscles, increasing the risk of incontinence. Maintaining a healthy weight through a balanced diet and regular exercise may help reduce this risk.
-
Stay Hydrated: While it may seem counterintuitive, staying hydrated is essential for bladder health. Drinking an adequate amount of water helps maintain a healthy urinary system and prevents urinary tract infections (UTIs), which can contribute to incontinence.
-
Avoid Bladder Irritants: Limiting or avoiding foods and drinks that irritate the bladder, such as caffeine, alcohol, carbonated beverages, and acidic or spicy foods, may reduce the risk of incontinence.
-
Practice Good Bathroom Habits: Avoid holding in urine for extended periods and respond promptly to the urge to urinate. Emptying the bladder regularly and completely can help maintain bladder health.
-
Regular Exercise: Engaging in regular physical activity can help improve overall muscle tone, including the pelvic floor muscles, which support bladder control.
-
Quit Smoking: Smoking can irritate the bladder and increase the risk of chronic coughing, which can contribute to stress incontinence. Quitting smoking can have a positive impact on bladder health.
-
Manage Chronic Conditions: Properly managing conditions such as diabetes, chronic cough, or constipation can reduce the risk of urinary incontinence.
-
Avoid Straining: Avoid straining during bowel movements, as this can put pressure on the pelvic floor muscles and affect bladder control.
It’s important to note that while these prevention strategies may be beneficial, urinary incontinence can still occur due to various factors, including genetics and hormonal changes. If someone experiences symptoms of urinary incontinence or has concerns about their bladder health, it’s essential to consult a healthcare professional for a proper evaluation and personalized advice on prevention and management strategies. Additionally, QMe offers packages support for various medical services and features automated billing to ensure transparent and hassle-free financial transactions. Embracing QMe empowers hospitals to enhance patient experiences, optimize healthcare workflows, and deliver top-notch medical services.
- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer