- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer
Bladder Cancer
Beyond the Horizon: Unravelling Bladder Cancer’s Mysteries and Breakthroughs
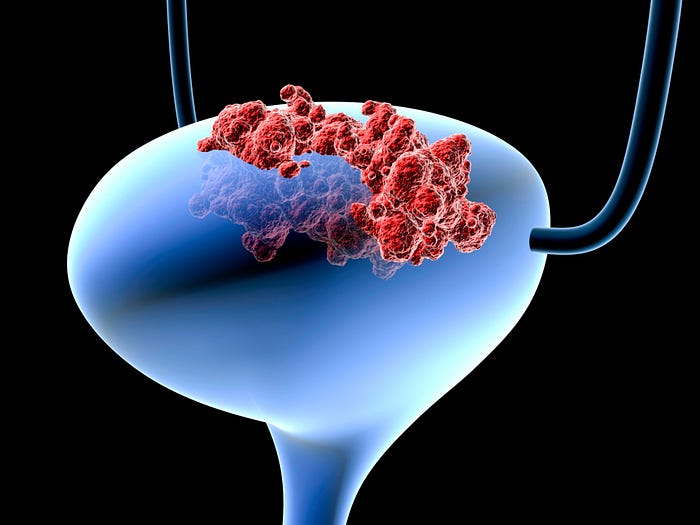
Bladder Cancer
Bladder cancer, a prevalent urological malignancy, originates in the tissues of the bladder lining. Its prevalence continues to pose a challenge to healthcare systems around the world due to a complex combination of hereditary and environmental factors. Urinary urgency and hematuria are typical symptoms. Classification comprises non-muscle invasive (NMIBC) and muscle-invasive (MIBC) types, each demanding distinct management approaches. Staging is aided by diagnostic tools like cystoscopy and imaging. Healthcare Treatment options range from transurethral resection and intravesical therapy for NMIBC to radical cystectomy and immunotherapy for MIBC. Current research explores innovative immunotherapies and tailored therapy, promising better results. This article explores the bladder cancer landscape while highlighting crucial elements in its comprehension and treatment.
Types and Classification of Bladder Cancer

Bladder cancer manifests primarily as non-muscle invasive (NMIBC) and muscle-invasive (MIBC) forms. NMIBC includes papillary urothelial neoplasms and carcinoma in situ (CIS), often treatable through transurethral resection and intravesical therapy. In contrast, MIBC, encompassing urothelial, squamous cell, and adenocarcinoma, presents higher risks and demands aggressive treatments like radical cystectomy. Rare histological types also exist. A precise classification is essential for choosing the best therapeutic approaches since MIBC demands comprehensive measures to provide the best possible outcomes for patients while NMIBC necessitates close monitoring to prevent progression and recurrence.
Risk Factors for Bladder Cancer

Bladder cancer risk factors comprise a blend of modifiable and non-modifiable elements. Foremost among these is tobacco exposure, notably smoking, accounting for a significant proportion of cases. Risk is also increased by workplace dangers such exposure to carcinogens and industrial chemicals. Chronic bladder inflammation and infections contribute, along with genetic predisposition and advancing age. Gender disparities are observed, with men being more susceptible. Understanding these risk factors makes it easier to establish focused prevention plans and screening programs, improving early identification and proactive bladder cancer therapy.
Symptoms and Diagnosis

Bladder cancer often presents subtle symptoms, such as hematuria (blood in urine) and lower urinary tract symptoms like urgency and frequency. Diagnosis requires a variety of methods. Direct visibility is made possible via cystoscopy, which makes tissue sampling and biopsy easier. Imaging like CT scans and ultrasounds aid staging. The coordination of various diagnostic methods, which guarantees correct assessment and prompt intervention, is crucially dependent on hospital administration. Early detection is essential for optimal treatment planning, underscoring the critical function of hospitals in providing all-encompassing care and enhancing outcomes for bladder cancer patients.
Staging and Prognosis
Bladder cancer staging, typically assessed using the TNM system, categorizes tumor size, lymph node involvement, and metastasis extent. Prognosis hinges on these factors, with higher stages indicating poorer outcomes. Healthcare management is essential in organizing staging tests like pathology and imaging, which helps determine the prognosis with accuracy. While bladder cancer in its early stages typically has a good prognosis, advanced stages necessitate extensive procedures. The ability to customize treatment programs is given to medical teams through timely and accurate staging, which improves patient outcomes and quality of life.
Treatment Options
Non-muscle invasive bladder cancer
1. Transurethral resection of bladder tumor (TURBT)
Transurethral resection of bladder tumor (TURBT) is a cornerstone procedure in non-muscle invasive bladder cancer management. Conducted under anesthesia, it involves inserting a cystoscope through the urethra to visualize and remove abnormal tissue growths. TURBT allows for precise tissue sampling for histopathology and tumor removal, serving both diagnostic and therapeutic objectives. The process assists in identifying the tumor’s grade and stage, which affects subsequent therapy choices. TURBT’s minimally invasive nature often allows for same-day discharge, facilitating swift recovery. TURBT allows for precise tissue sampling for histopathology and tumor removal, serving both diagnostic and therapeutic objectives. The process assists in identifying the tumor’s grade and stage, which affects subsequent therapy choices.
2. Intravesical therapy (immunotherapy, chemotherapy)
An area-specific strategy for the non-invasive treatment of bladder cancer is intravesical therapy. It entails inserting a catheter directly into the bladder to deliver therapeutic drugs like immunotherapy or chemotherapy. Immunotherapy activates the immune system to target cancer cells, frequently using Bacillus Calmette-Guérin (BCG). Cell proliferation is inhibited by chemotherapy. Following transurethral resection, these therapies work to eliminate any cancer cells that remain and stop the disease’s growth and recurrence. Weekly sessions help to increase effectiveness. Among the negative effects is bladder discomfort. Tailoring the therapy to patient needs is essential. Intravesical treatment is essential for maintaining bladder function and preventing disease recurrence.
Muscle invasive bladder cancer
1. Radical cystectomy
An essential medical treatment for bladder cancer that has spread to the muscles is radical cystectomy. If necessary, the surrounding organs, lymph nodes, and bladder are surgically removed. This intricate procedure necessitates considerable surgical skill and cross-disciplinary collaboration. In men, prostate removal, and in women, uterus and ovaries removal may be included. Post-surgery, patients often require reconstructive procedures like neobladder or ileal conduit creation to manage urine elimination. The preoperative evaluation, surgical execution, and postoperative care performed by healthcare teams are essential to maximizing patient outcomes and quality of life following radical cystectomy.
2. Neoadjuvant and adjuvant therapies
Neoadjuvant therapies are administered before the main treatment, like chemotherapy before radical cystectomy in muscle-invasive bladder cancer. They reduce tumor size, making surgery easier. Adjuvant therapies are given after the primary treatment to target any remaining cancer cells. For bladder cancer, adjuvant chemotherapy or immunotherapy might follow surgery to enhance treatment efficacy and reduce the risk of recurrence and metastasis. These multimodal strategies attempt to enhance patient outcomes and are essential to comprehensive cancer care.
Advanced and metastatic bladder cancer
1. Chemotherapy
Chemotherapy for bladder cancer involves administering anti-cancer drugs systematically, either orally or intravenously. It interferes with the growth and spread of cancer cells by targeting those that divide quickly. It can decrease tumors in severe situations, improving the efficacy of surgery or other treatments. Chemotherapy has a number of negative side effects, including weakness in the immune system, exhaustion, and nausea. Plans for treatment are made specifically for each patient and could involve multiple therapy. Supportive care and routine monitoring are crucial elements of chemotherapy management.
2. Immunotherapy (checkpoint inhibitors)
Checkpoint inhibitor immunotherapy is a novel strategy for treating bladder cancer. These medications target particular immune response-regulating proteins, freeing the brakes on immune cells and enhancing their capacity to discover and combat cancer cells. In situations of advanced bladder cancer that don’t respond to conventional therapies, checkpoint inhibitors like pembrolizumab and atezolizumab have demonstrated notable success. While generally well-tolerated, side effects can occur, including immune-related adverse events. Individualized treatment programs and routine monitoring are crucial. A promising approach to redefining bladder cancer management is immunotherapy.
3. Targeted therapies
Targeted therapy for bladder cancer concentrates on particular molecules involved in the development and spread of the disease. These medications stop the signals that promote tumor growth or reduce the blood flow to tumors, which impedes tumor growth. Targeted therapies, as opposed to conventional chemotherapy, attempt to protect healthy cells and lessen side effects. The effectiveness of these medicines in treating bladder cancer is increased by customized therapy regimens based on molecular traits.
Emerging Therapies and Research

New treatments and ongoing research into bladder cancer are pursuing novel directions under the direction of organizations like QMe HMIS. Based on genetic profiles, personalized medicine develops treatments specifically for each patient, improving accuracy and results. Novel immunotherapies, beyond checkpoint inhibitors, are under scrutiny, promising enhanced immune responses. For early detection, prognosis, and the prediction of therapy response, biomarkers are being studied. Among other research organizations, QMe HMIS is essential to understanding these developments. Collaboration among scientists, medical professionals, and patients guarantees that these discoveries are translated into practical clinical approaches, ushering in a new era in the treatment of bladder cancer.
Supportive Care and Quality of Life
Along with medical treatments, supportive care is crucial in the management of bladder cancer, concentrating on improving patients’ quality of life. Healthcare professionals provide methods for controlling the adverse effects of treatment, reducing pain, and addressing psychosocial issues. Plans for fitness and dietary advice enhance overall wellbeing. The emotional toll of the condition can be managed with the help of psychological treatment. Patients with advanced cancer are given comfort through palliative care, which is offered by medical teams. The promotion of holistic care by incorporating these factors into healthcare management places an emphasis on patients’ comfort, emotional fortitude, and dignity throughout their bladder cancer journey.
Prevention and Public Health
Smoking cessation programs
Smoking cessation programs are essential interventions meant to aid smokers in quitting. To help people overcome their nicotine addiction, these programs provide counseling, behavioral support, and occasionally medicine. Such programs are essential for public health and disease prevention since quitting smoking considerably lowers the risk of bladder cancer and improves general health.
Occupational safety measures
Implementing protocols to protect employees from hazardous exposures in diverse industries is a part of occupational safety measures. These precautions include appropriate training, the use of safety gear, and adherence to protocols while working with carcinogenic compounds in the context of preventing bladder cancer. A safe workplace reduces the danger of chemical exposure, which lowers the chance of bladder cancer and other occupational health problems.
Education and awareness campaigns
Raising public awareness of bladder cancer dangers, symptoms, and prevention requires effective education and awareness programs. These initiatives spread knowledge about early detection and healthy lifestyle choices using a variety of channels, including social media and local events. Education and awareness initiatives dramatically reduce the burden of bladder cancer and support pro-active healthcare practices by empowering people to detect the symptoms and adopt preventive measures.
Conclusion
In conclusion, thorough methods to prevention, diagnosis, and therapy are required given the complex nature of bladder cancer. The importance of effective healthcare management is shown by QMe Hospital Management and Information Systems’s role in orchestrating seamless care, from diagnostics to therapeutic actions. Advanced information software also helps to streamline patient data, enable individualized therapies, and facilitate scientific breakthroughs. As science develops, targeted approaches, immunotherapies, and personalized therapeutics have the potential to transform the way bladder cancer is managed. Patient comprehension and coping mechanisms are enhanced by education, awareness campaigns, and support systems. We ultimately hope to improve outcomes, improve quality of life, and advance the fight against bladder cancer through cooperative efforts of healthcare organizations, patients, and researchers.
- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer